Complex thoracic aortic disease poses a significant threat to life and demands highly skilled surgical management. This condition affects the upper portion of the aorta, the main artery that transports blood from the heart to the rest of the body. When this area becomes weakened or diseased, prompt and strategic intervention becomes essential. With significant advancements in cardiovascular surgery and technology, specialists now have a wide range of tools and techniques to address even the most complex thoracic aortic cases effectively.
Understanding the Nature of Complex Thoracic Aortic Disease
The term complex thoracic aortic disease refers to several life-threatening conditions that affect the thoracic segment of the aorta. These include thoracic aortic aneurysms, dissections, penetrating ulcers, and intramural hematomas. What makes them complex is their size, shape, or involvement of adjacent aortic branches and vital organs. These diseases may be asymptomatic at first, but if untreated, they can lead to catastrophic rupture or organ damage.
Most patients develop these issues due to aging, high blood pressure, genetic disorders like Marfan syndrome, or a history of smoking. Imaging techniques, such as CT angiography or MRI, help doctors identify these conditions early and make informed decisions about the timing and method of repair.
Surgical Techniques Shaping Patient Outcomes
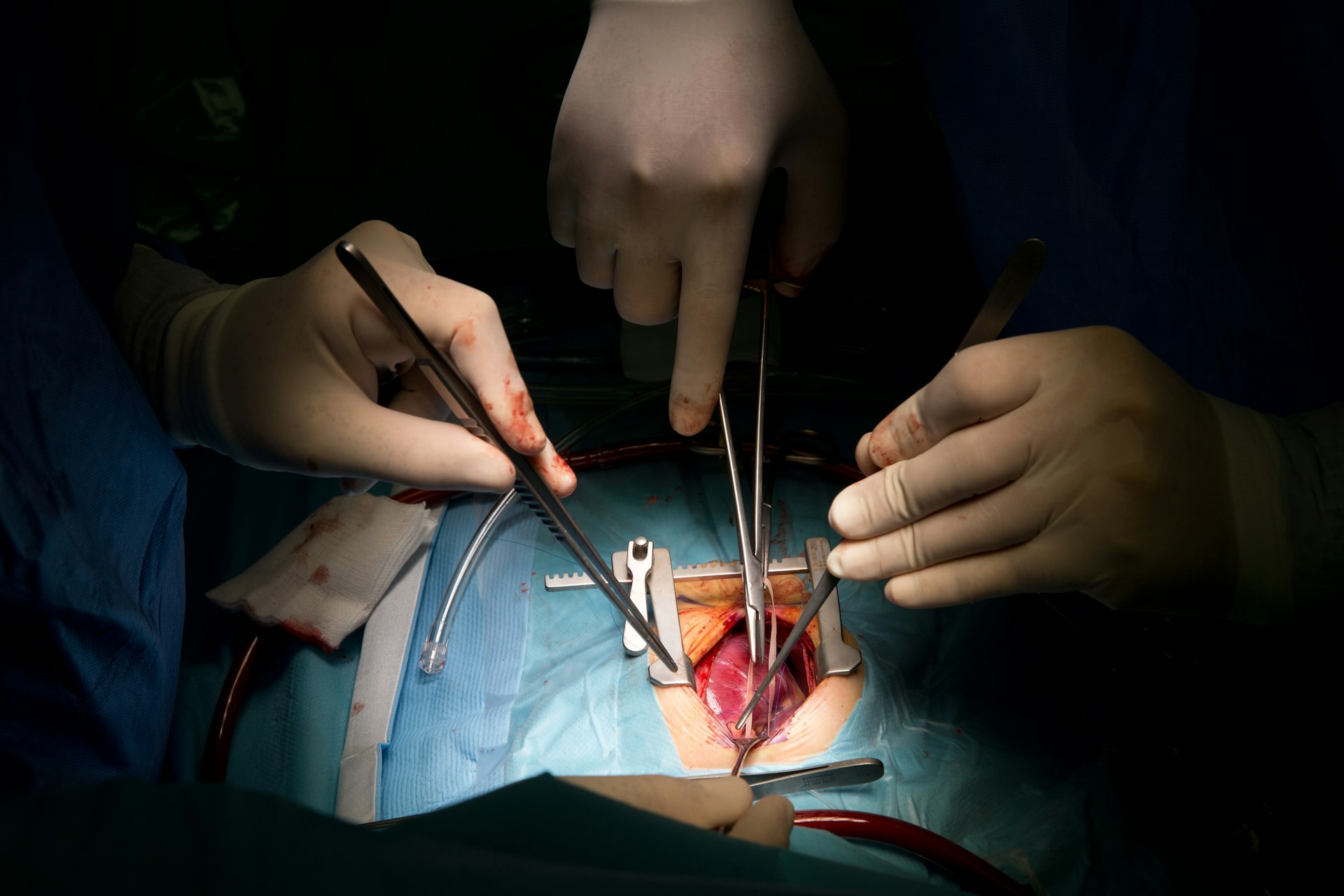
The surgical management of thoracic aortic disease has advanced significantly in recent years. For many patients, open aortic repair remains the gold standard, especially when the anatomy is not suitable for less invasive options. This approach involves replacing the diseased section of the aorta with a synthetic graft, and it often requires cardiopulmonary bypass and hypothermic circulatory arrest for safe performance.
However, not all patients are good candidates for open surgery. In such cases, thoracic endovascular aortic repair (TEVAR) offers a less invasive and often safer alternative. TEVAR involves delivering a stent graft through the femoral artery and deploying it within the diseased segment to reinforce the aortic wall. It significantly reduces recovery time and is especially helpful for elderly or high-risk individuals.
More recently, hybrid approaches have emerged, blending the benefits of open and endovascular repair. Surgeons might first reroute aortic branches surgically and then use TEVAR to fix the diseased portion. This method proves highly effective for patients with arch or descending aortic disease involving critical branches.
Challenges Surgeons Face in Treating Complex Cases
Surgical care for complex thoracic aortic disease is not without its challenges. First, precise timing is critical. Intervening too early may expose the patient to unnecessary risk while waiting too long increases the chance of rupture. Second, access to the aorta in the chest cavity requires advanced surgical skills and is best achieved in high-volume centers with specialized experience.
Another hurdle is the risk of spinal cord ischemia. The aorta supplies blood to the spinal cord, and interrupting that supply can lead to paralysis. Surgeons must carefully preserve blood flow during the procedure, often using spinal drains and neuro-monitoring to minimize this risk.
Patients with connective tissue disorders or a history of aortic surgery also add complexity to the planning. In such cases, each intervention must be part of a larger, staged plan tailored to the individual’s anatomy and overall health status.
Innovations Improving Surgical Outcomes
Technology has significantly improved the way surgeons handle complex thoracic aortic disease. Preoperative planning now relies on 3D reconstructions and advanced imaging software that help map out the entire aorta and its branches. This enables more accurate graft sizing and positioning, thereby minimizing complications.
Custom-made stent-grafts, especially in TEVAR, are another game changer. These devices can be designed to fit a patient’s exact anatomy, which is especially useful when treating aortic arch disease. Moreover, new materials and designs have enhanced durability and flexibility, providing surgeons with more reliable tools.
Additionally, enhanced intraoperative imaging, such as transesophageal echocardiography and intraoperative angiography, enables real-time visualization during surgery, yielding safer procedures and improved outcomes.
Multidisciplinary Collaboration Drives Better Results
No single specialist can handle complex thoracic aortic disease alone. Today’s best outcomes result from teamwork. Cardiothoracic surgeons, vascular surgeons, interventional radiologists, anesthesiologists, and cardiologists collaborate to ensure that patients receive comprehensive care.
Multidisciplinary aortic centers have proven particularly effective in managing these cases. These centers bring together all necessary expertise in one location, enabling rapid diagnosis, immediate risk assessment, and customized surgical planning. Patients benefit from fewer complications, shorter hospital stays, and improved survival rates.
The care continues after surgery, with close follow-up through imaging and blood pressure management. Surveillance ensures that any changes in the remaining aorta are caught early, allowing for timely intervention if needed.
Looking Ahead: The Future of Thoracic Aortic Surgery
The future holds exciting promise for those facing complex thoracic aortic disease. Research into bioengineered grafts, which can grow and adapt with the patient, may eventually eliminate the need for multiple surgeries in younger individuals. Artificial intelligence is also beginning to play a role in surgical planning, helping identify the best strategies for each patient.
As more hospitals invest in advanced aortic centers and training programs, access to life-saving care will expand. Moreover, public awareness about the signs and risks of thoracic aortic disease—such as chest pain, shortness of breath, or back pain—can lead to earlier diagnoses and improved chances of recovery.
The integration of real-time monitoring, improved anesthesia techniques, and post-operative rehabilitation programs will continue to shape a more holistic, patient-centered approach. Personalized medicine, where treatments are tailored to each patient’s genetic and health profile, may soon guide both prevention and intervention strategies.
Surgical management of complex thoracic aortic disease has evolved into a highly specialized and collaborative effort. With innovations in open repair, endovascular techniques, and hybrid methods, surgeons now have more options than ever to treat this deadly condition. The shift toward team-based care and technological advancement continues to improve survival rates and quality of life for affected patients.
As we look to the future, the combination of research, innovation, and expert collaboration promises to transform further the care of individuals with complex thoracic aortic disease. Early diagnosis, proper planning, and experienced surgical teams remain the foundation of successful outcomes in this challenging but increasingly manageable field.